 Chronic Obstructive Pulmonary Disease (COPD: obstructive; to block and pulmonary; lung) is a group of lung diseases that hamper your ability to breathe normally; partially blocking your airways. COPD is progressive with the symptoms getting worse over time and is irreversible. The longer you have COPD, the harder it is to breathe. COPD is a major cause of disability and decreased quality of life, impacting your work, time with family and the most basic and simple pleasures of a normal life.
Chronic Obstructive Pulmonary Disease (COPD: obstructive; to block and pulmonary; lung) is a group of lung diseases that hamper your ability to breathe normally; partially blocking your airways. COPD is progressive with the symptoms getting worse over time and is irreversible. The longer you have COPD, the harder it is to breathe. COPD is a major cause of disability and decreased quality of life, impacting your work, time with family and the most basic and simple pleasures of a normal life.
About
How a Normal Lung Works
Airways are tubes that carry air in and out of the lungs through the nose and mouth. Healthy lungs are open and elastic, which allows small sacs (called alveoli) to fill up with air.
What Happens When You Have COPD?
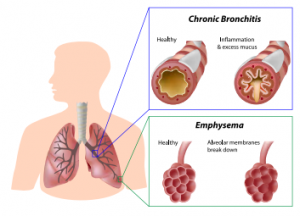
COPD causes the airways to swell, which may shut off small airways and narrow larger ones. Additionally, the airways can become clogged with mucus, making breathing even more difficult. When you inhale, air goes into your lungs, but narrow or blocked airways make it difficult for air to leave when you exhale. There are two main forms of COPD. You can have just one of them, but most people develop both at the same time.
Chronic Bronchitis (bron-KY-tus):
Chronic bronchitis is a cough that occurs every day for at least 3 months, 2 years in a row. This happens when your bronchial tubes (the tubes that are the pathways for air in and out of the lungs so you can breathe) are inflamed and less air is able to flow through to your lungs causing you to cough up mucus or phlegm.
Emphysema (em-fuh-ZEE-muh):
This is when the walls of the air sacs (alveoli) in your lungs break down causing the air spaces to enlarge, trapping the air. As emphysema gets worse it tranforms the air sacs — which normally look like a bunch of grapes — into large, irregular pockets with gaping holes in their inner walls, reducing the amount of oxygen that reaches your bloodstream. Although COPD is a lung and breathing disease, it can also make it harder for your heart to efficiently pump blood throughout your body, which can lead to high blood pressure and in some extreme cases, to heart failure.
RISK FACTORS
There are three major risk factors and several smaller ones. Let’s go through them in order of importance:
- Smoking. This is by far the most significant risk factor. Between 80 – 90% of people diagnosed with COPD are over 40 years old and either smoke now or did smoke. In addition, 90% of COPD-related deaths occur in current or former smokers. The more cigarettes you smoked and the longer you smoked, the worse your symptoms will be. And while cigarettes cause most cases of COPD, many people with the disease also smoke (or smoked) pipes, cigars, and/or marijuana, or had long-term exposure to second-hand smoke.
- Air quality. If you’ve worked in a place where you’ve had long-term exposure to things that can irritate your lungs, such as chemicals, strong fumes, or dust, you’re more likely to develop COPD. If you are or were a smoker, your risk is even higher. But even if you never smoked, this kind of occupational exposure significantly increases your risk, as does long-term exposure to very high levels of air pollution.
- Genetics. People with a deficiency of alpha-1-antitrypsin (AAT)—a protein produced by the liver—are more likely to develop emphysema. Smoking adds to the risk but AAT deficiency increases COPD risk in people who have never smoked or been exposed to toxic chemicals, dust, fumes or polluted air—regardless of their age. About 100,000 Americans have an AAT deficiency; most are of Northern European descent. There is also some evidence that having a sibling or other close relative with COPD may increase your risk.
- Asthma. Some research shows that people with asthma may have a much higher risk of developing COPD—even if they don’t smoke.
- Childhood lung infections. If you had a severe lung infection when you were a child, your lungs may not function as well as those of someone who didn’t. Decreased lung function may make you more susceptible to COPD.
COPD’s Effect on Sexual Health
COPD symptoms like coughing, wheezing, and shortness of breath may change the way you and your partner enjoy sex. For those with COPD fear of shortness of breath during times of sex can lead to avoidance of sex. They may be unable to maintain sexual arousal or reach climax. The non-COPD partner may also be less inclined toward sex, thinking it to be in the best interest of the COPD partner.
You can still have sex or partake in other forms of physical intimacy. If you’re worried about shortness of breath or wheezing after exertion, try other activities to increase oxygen flow in the blood. This will get your body accustomed to the exertion. If you’re able to walk up 2 flights of stairs without being too winded then you should be able to perform sexually. Keep consistent with taking prescribed medications.
- Talk to your provider if you are noticing erectile/performance symptoms that may be related to medications.
- If you use an inhaler for respiratory issues, make sure to have it nearby.
- Avoid sex immediately after a large meal.
- If on supplemental oxygen, extend the tube leading to the tank and keep it nearby.
The important thing is to speak with your partner when you are having symptoms and might need a break during intercourse. Difficulty breathing and coughing can make people with COPD feel very tired and depressed. Your partner may feel anxious or frustrated about the breathing problems. It is important to talk about your worries together. COPD may diminish frequency or duration of sex, but doesn’t affect ability.
FYI
- COPD is the 3rd leading cause of death in the U.S. (heart disease and cancer are numbers 1 and 2)
- COPD kills approximately 120,000 men and women each year
- About 12 million Americans have been diagnosed with COPD and as many as 12 million more may be suffering from the disease but don’t know they have it
- Approximately 85 – 90% of COPD deaths are caused by smoking
- Every four minutes an individual dies of COPD
CARING FOR SOMEONE WITH COPD
If a loved one has COPD, talk to their healthcare provider about how you can prepare yourself and your home to make it more livable for them. You will have to keep track of medications, attend medical appointments and help your loved one manage symptoms.
- If you have stairs he or she may be unable to climb them, so set up a place to sleep on the first floor. Add safety bars around the house, especially in the bath tub and near the toilet.
- Prepare a journal so you can track medications, their doses, and administration times.
- Beware of infections. People living with COPD are at risk of catching colds and flu. For a person with COPD, a chest infection can lead to hospitalization.
- People living with COPD often have flare-ups, which can lead to hospitalization. For more information on flare-ups, their symptoms and steps you can take to prevent them from occurring, take a course in cardiopulmonary resuscitation (CPR). It could come in handy.
- Speak to your healthcare provider about enrolling the patient in a pulmonary rehabilitation program.
- COPD can make people feel very anxious and depressed. They may become irritable, afraid of being left alone, and frustrated that they can’t do things like they used to. It’s important that you give them lots of reassurance, show plenty of support, and keep an eye out for signs of depression.
- Provide a healthy diet that’s low in saturated fats and high in whole grains, fruits and vegetables. A healthy diet is essential.
- If you or anyone in your home smokes, it’s time to quit now
When to Call 9-1-1
Knowing when your partner is in need of emergency treatment can be stressful. If he or she is complaining of more symptoms than usual, or if you notice any of the following symptoms, pick up the phone and call 9-1-1.
Call 9-1-1 if your loved one:
- Stops breathing
- Is gasping, having difficulty speaking, or is much more short of breath than usual
- Experiences severe chest pain or chest pain is quickly getting worse
- Develops a high fever {over 101°F (38.3°C)}
- Shows any flu-like symptoms
Here are some other important steps you can take to help yourself as you manage your loved one’s condition:
- Educate yourself. The more you know about the illness, the more effective you will be in your care.
- Provide your loved one with encouragement, celebrate improvements and let them do as much as possible independently.
- Stay organized. Unexpected bills can pile up quickly, whether or not you have health insurance, Medicare, or are on Medicaid. Communicate with your insurance company or healthcare provider immediately and take appropriate action. Speak to the patient services department at your hospital to determine your options.
- Join a caregiver support group. Sharing your feelings and experiences with others in the same situation can help you manage stress and reduce feelings of frustration and/or isolation.
- Don’t forget to take care of yourself too. Make sure you eat regular healthy meals and get plenty of rest.
YOUR PARTNER: WOMEN AND COPD
COPD is not only a man’s disease. COPD in women has been increasing. In fact, today, more women than men die from COPD.
The major risk factor for developing COPD is smoking, and female smokers are much more likely to die from COPD than women who have never smoked. Research has also shown that the effects of smoking actually have a greater impact on women’s lung health than men’s and they tend to report worse symptoms than men for similar severity of COPD. This is mainly due to the fact that women have smaller lungs and airways, and therefore tend to develop COPD at lower smoking levels than men.
Compared to men, women with COPD experience:
- More severe shortness of breath
- Higher rates of depression
- More anxiety
- More frequent exacerbations (flare-ups)
- Lower quality of life because of the misconceptions about COPD, women are also less likely to be correctly diagnosed or offered appropriate diagnostic tests for COPD by healthcare providers. If your partner has difficulty breathing, whether she’s a smoker or not, encourage her to go see her healthcare provider.
Because of the misconceptions about COPD, women are also less likely to be correctly diagnosed or offered appropriate diagnostic tests for COPD by healthcare providers. If your partner has difficulty breathing, whether she’s a smoker or not, encourage her to go see her healthcare provider.
Symptoms
In the early stages, the symptoms of COPD can be so mild that you may not notice them. Or if you did notice them, you might have brushed them off as “no big deal” or “it’s just part of getting older.” Some people even develop workarounds to make the symptoms less of an inconvenience. For example, some people who find themselves breathing hard after going up a flight or two of stairs may start taking the elevator more often. Although that might make the symptoms go away, the underlying problem is still there. As with any health issue, it’s important to pay attention to your body.
Here are the symptoms to look out for:
- Shortness of breath (called dyspnea). You may feel like breathing is hard work and that you can’t seem to get enough air. This happens especially when you exercise, but it can even happen when you’re doing something as simple as taking groceries out of the car or going for a walk around the neighborhood.
- Chronic cough. This is when you have a constant cough that produces a lot of mucus (often called “smoker’s cough”). This means that your body is trying to get rid of excess mucus, debris (such as dust), or irritants (such as cigarette smoke).
- Wheezing. Making a whistling sound when you inhale or exhale is usually a sign that your airways are so blocked that air is hardly getting through.
- Chest Tightness. Feeling like you can’t breathe or take a deep breath.
Not every person who has these symptoms has COPD and not every person with COPD has these symptoms. However, if you think you have any of the symptoms we have discussed here, the safe thing to do is to see your healthcare provider and let him or her make a diagnosis.
What is an exacerbation? (ig-zas-er-BAY-shun)
This means that your symptoms get worse and worse and last for a few days. This can happen suddenly. Most of the time, exacerbations are caused by bronchitis, pneumonia, or some other infection, virus, or bacteria in the lungs. This is definitely one of those “you-know-it-when-you-see-it” kinds of things.
If you don’t take steps to treat your COPD (see Treatment section) your symptoms will get worse and you may have a COPD flare-up also known as exacerbation. During a flare-up, you may:
- Cough or wheeze more often and for longer periods
- Find it so hard to breathe that you can’t walk or talk without gasping
- Purse your lips when you breathe. That’s another sign that you’re having to work really hard to get air in and out.
- Notice that your fingernails, lips, and sometimes even your skin are turning blue. This is the result of not getting enough oxygen to your body.
- Cough up more mucus than usual or the mucus you cough up might become darker and thicker.
- Cough up blood. This is never a good sign. If you haven’t done so already, you need to call your healthcare provider right now.
- Lose weight. For some people with COPD, breathing is so difficult that they actually burn off more calories inhaling and exhaling than they take in through their food.
- Have swelling in the ankles, feet, and legs
- Have a fever
Prevention
- Make sure your employer provides adequate ventilation as well as masks, air filters, and other personal protective equipment.
- Stay away from backyard barbeques and indoor fireplace fires or wood-burning stoves.
- Stay away from places where there’s likely to be dust, cigarette smoke or any other irritants.
- Watch for mold. Mold occurs when your home has too much moisture, and it draws into the general ventilation system, worsening air quality. To prevent mold, install an air filter, try running an air conditioner or keeping a dehumidifier, especially in the basement.
- When cleaning, try to use natural products that are less likely to irritate your lungs than bleach and other harsh chemicals.
- Finally, pay close attention to radio and TV public service announcements about air quality and stay inside when the air outside is especially polluted. If you cannot avoid air pollution, wear an air pollution mask to minimize your exposure
TAKE ACTION: LIFESTYLE CHANGES
Whether you need medical intervention or not, we recommend that you make the following lifestyle changes. This will make you feel better in the long run.
Quit smoking. If you’re a smoker, quitting is by far the best thing you can do. If you’re having trouble quitting on your own, talk to your healthcare provider about prescription options, which may include patches, gum or prescription medication.
Stay active. Regular exercise will help improve your COPD symptoms. Talk to your healthcare provider about how much physical activity and what kinds of activities are best for you. These might include stretching exercises, aerobic exercise like walking, or exercises aimed at strengthening your muscles.
Stay healthy. The flu is never a good thing, but for people with COPD it could be deadly. The same goes for pneumonia. Speak to your healthcare provider about getting a flu shot and/or a pneumonia vaccine. In addition, take other steps to stay healthy such as washing your hands frequently to remove germs, and if possible, staying away from crowds and sick people.
Watch out for air quality. When you have COPD, the key is to prevent flare-ups. Stay away from indoor and outdoor air pollution, cold dry air, hot humid air and high altitudes.
Eat healthy. When you have COPD, you may feel too tired to eat properly and this can lead to muscle weakness and weight loss. It’s important that you eat healthy, well-balanced meals as this will give you much-needed energy and strengthen your immune system.
Diagnosis
HOW IS COPD DIAGNOSED?
Depending on your symptoms, there are several ways your healthcare provider may diagnose COPD.
- Spirometry. This simple, non-invasive, painless test is given to all patients who show symptoms of COPD. During the test, your healthcare provider will ask you to take in a deep breath. Then, you will blow out as hard as you can into a tube that’s connected to a small machine. The machine will measure how much air you can blow out of your lungs and how quickly you can do it. Based on the results of the test, your provider will be able to tell whether or not you have COPD and if so, how severe it is.
Other tests include:
- Bronchodilator reversibility. During this test, you’ll be given a type of lung medication called a bronchodilator, which will help relax your breathing muscles so you can breathe more easily. The amount of improvement in your breathing after taking the bronchodilator will help your healthcare provider diagnose lung problems or monitor the status of an existing lung condition.
- Chest X-ray. This will provide a picture of your heart and lungs. This test alone will not diagnose COPD but it will enable your healthcare provider to assess how far your COPD has advanced. It will also help your healthcare provider rule out other conditions that might be causing your breathing problems, such as lung cancer, heart failure, pneumonia or tuberculosis.
- Arterial blood gas analysis. This blood test measures how well your lungs are sending oxygen throughout your body. The blood is usually drawn from an artery in your wrist. This will let your healthcare provider assess whether or not you need oxygen therapy
Questions to Ask Your Health Care Provider
- What is causing my COPD?
- Does my condition involve emphysema, chronic bronchitis, or a combination of these conditions?
- What will make my COPD worse?
- What treatment options are best for me? Will I need oxygen?
- What are the benefits/side effects of the medications you prescribe?
- Are there any alternative or complementary therapies that will help me feel better?
- Are there dietary changes I should make? How do I go about it?
- Will I still be able to work and participate in activities?
- What lifestyle changes can I make at home to help reduce my symptoms?
- What are some signs that my breathing is getting worse and that I should call the healthcare provider? What should I do when I feel I’m not breathing well enough?
- How often do I need to come in for check-ups?
Treatments
TREATMENT OPTIONS
Unfortunately, there is no cure for COPD. The goal is to keep your symptoms from getting any worse and to improve the quality, even the length, of your life. This may include one or more of the following:
- Medication. There are a variety of prescription drugs that are very successful in treating coughing and wheezing. Some medications work by relaxing the muscles around your airways, which makes it easier to breathe. Others work by helping keep the airways from getting inflamed in the first place. Not all medications are appropriate for everyone, so make sure to take only the ones your healthcare provider prescribes, and that you take them as directed.
- Pulmonary rehabilitation. During this program, healthcare specialists will teach you specific exercises and disease management techniques to help you manage your symptoms, increase overall strength, and improve your lung function. This is especially important if you are having trouble completing your daily activities and chores.
- Oxygen. If your COPD is severe, your healthcare provider may prescribe supplemental oxygen. Depending on your symptoms, you may need oxygen all the time or you may be able to get by with occasional boosts. Getting this extra oxygen will slow down the progression of the disease and will most likely allow you to do activities that you hadn’t been able to do for a while because breathing was so hard.
- Surgery. Patients with the most severe COPD who do not respond to prescribed medications may require surgery to improve their lung function. In some extreme cases, as a last resort, a lung transplant may be required