Hypogonadism (hi-po-go-na-dizm) also known as low testosterone (Low T), occurs when the body does not produce enough male sex hormones (androgen deficiency), specifically testosterone, and it can result in sexual impotence, infertility, loss of muscle mass and strength, reduction in bone density, mood changes and fat accumulation. It can develop from a testicular disorder at any age or it can result from disease, injury or drug abuse.
About
There are two basic types of male hypogonadism, which both result in decreases in sperm and testosterone production.
Primary hypogonadism is low testosterone due to a dysfunction or defect in the testes.
Secondary hypogonadism is low testosterone due to a dysfunction or defect in the pituitary gland or hypothalamus (the parts of the brain that signal the testicles to produce testosterone).
What is Testosterone?
Testosterone is the most important sex hormone in the male body. It is needed for masculine growth and development during puberty, and the development of male characteristics such as body and facial hair, muscle growth, strength and a deep voice. Normal levels of testosterone also influence the production of sperm, promote sexual function and sex drive. The brain and the testicles work together to keep testosterone levels within a normal range. When levels of testosterone are below normal, the brain signals the testicles to make more. When testosterone levels are too high, the brain signals for the testicles to make less.
FYI
TESTOSTERONE & AGING
The ability to produce testosterone declines as men age, resulting in a condition called hypogonadism or Low Testosterone (Low T). This loss of testosterone may lead to uncomfortable and distressing symptoms. Researchers estimate that hypogonadism affects from 2-6 million men in the United States with only 5% receiving treatment.*
Low T may affect a man’s interest in sex, his ability to perform sexually and it can result in sexual impotence, infertility, loss of muscle mass and strength, reduction in bone density, mood changes and fat accumulation. Causes of Low T vary, and some men are born with the condition, while others develop it later in life. Low T is characterized by low levels of testosterone and presents such symptoms such as decreased sexual desire, erectile dysfunction, decreased energy and depression.
It’s normal for a man’s sex drive to slowly decline from its peak in his teens and 20s, but libido and sex drive vary widely among men and also for an individual over time. It is affected by stress, sleep, general health and opportunities for sex. Men may not recognize a problem until a partner considers it an issue or the man recognizes he cannot function sexually.
Symptoms
In Puberty: Hypogonadism may delay puberty or inhibit development. You may notice the following symptoms:
- Decreased development of muscle mass
- Lack of deepening of the voice
- Impaired growth of body hair
- Impaired growth of the penis and testicles
- Excessive growth of the arms and legs in relation to the trunk of the body
- Breast enlargement (gynecomastia)
In Adulthood: Hypogonadism may alter physical characteristics, cause health problems or impair reproductive function. You may notice the following symptoms.
- Erectile dysfunction and other sexual problems
- Infertility
- Decreased beard and body hair
- Decrease in muscle mass
- Breast enlargement (gynecomastia)
- Loss of bone mass (osteoporosis)
Some men may also experience the following signs and symptoms:
- Fatigue
- Decreased sex drive
- Difficulty concentrating
- Hot flashes
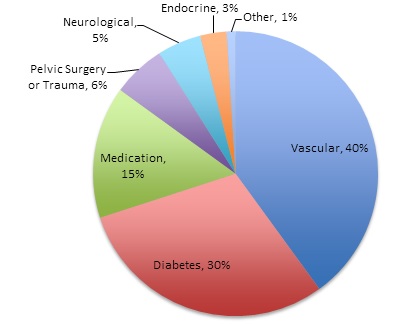
CAUSES OF HYPOGONADISM IN MEN INCLUDE:
- Obesity
- Certain medications
- Certain inflammatory diseases
- Injury or infection involving the testicles
- A genetic abnormality, such as Klinefelter’s syndrome, in which males have an extra “X” chromosome
- Undescended or absent testicles
- Iron overload (hemochromatosis)
- Cancer treatment, including radiation and chemotherapy
- Toxic damage from alcohol or heavy metals
- Congenital hormone disorders affecting the hypothalamus or pituitary gland, such as Kallmann’s syndrome
- HIV/AIDS
- Normal aging
Prevention
GET SCREENED
You may want to ask your healthcare provider to check you for low testosterone levels if you experience symptoms associated with Low T. A primary care provider checks testosterone levels with a blood test to determine if you have Low T and determine if testosterone therapy is right for you. You might also ask your healthcare provider about a referral to an endocrinologist or urologist who specializes in treating Low T.
Questions to Ask Your Health Care Provider
In order to get the best treatment, it’s important that you become a proactive partner in your healthcare. Here are some questions you can ask your healthcare provider about Low Testosterone.
- I don’t feel sick; I just don’t feel like myself anymore. What could be causing it?
- Are the symptoms I am experiencing and my other conditions related to Low T?
- What medical treatment options are available if I have Low T?
- What are the benefits/side effects of the medications you prescribe?
- Are there dietary changes I should make? How do I go about it?
- Will I still be able to work and participate in activities?
- What is the difference between the different testosterone replacement therapies?
- If I have Low T, what happens if I don’t have it treated?
- How often do I need to come in for check-ups?
Treatments
If you do experience symptoms of Low Testosterone and are diagnosed by a healthcare provider, the good news is that the condition very often is treatable.
There are several FDA-approved testosterone replacement therapies, including:
Gels and Solutions
Testosterone gels and solutions are applied directly to the skin and are absorbed into the body. These generally require daily application.
Patches
Patches allow testosterone to be absorbed by the skin. Patches are applied daily, typically to the back, abdomen, upper arm or thigh.
Injections
Testosterone injections, usually in the upper buttock, are typically given every 1-2 weeks. However, there are some long-acting injections that can be administered every 10 weeks.
Buccal Tablet
In your mouth, the tablet is applied to the gum, where testosterone is absorbed over a 12-hour period. They are taken twice daily.
Pellets
Pellets are implanted under the skin near the hip during a surgical procedure by a healthcare provider.
REMEMBER:
Regular checkups and age-appropriate screening, including low testosterone, can improve your health and extend your life.
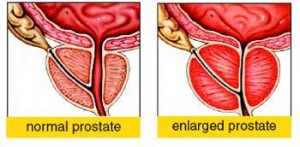
Testosterone therapy should not be used in men with carcinoma of the breast or known or suspected carcinoma of the prostate. Geriatric patients treated with androgens may be at an increased risk for the development of prostatic hyperplasia and prostatic carcinoma.
Resources
To learn more about Hypogonadism visit the following pages
Medscape
Cleveland Clinic
Medline Plus
What Men Should Know About Testosterone
The following professional and patient care organizations are available as resources for further information about low Testosterone and testosterone replacement therapy:
American Academy of Family Healthcare providers (AAFP)
11400 Tomahawk Creek Parkway
Leawood, KS 66211
913-906-6000
www.aafp.org
American Osteopathic Association (AOA)
142 E. Ontario St.
Chicago, IL 60611-2864
800-621-1773
www.osteopathic.org
American Association of Clinical Endocrinologists (AACE)
1000 Riverside Avenue, Suite 205
Jacksonville, FL 32204
904-353-7878
www.aace.com
American Society for Reproductive Medicine
1209 Montgomery Highway
Birmingham, AL 35216
205-978-5000
www.asrm.org
American Urologic Association (AUA)
1000 Corporate Boulevard
Linthicum, MD 21090
410-689-3700
www.auanet.org
The Endocrine Society
8401 Connecticut Avenue, Suite 900
Chevy Chase, MD 20815
301-941-0200
www.endo-society.org
The Hormone Foundation
8401 Connecticut Avenue, Suite 900
Chevy Chase, MD 20815
800-HORMONE
www.hormone.org
Sexual Medicine Society of North America, Inc.
1111 North Plaza Drive, Suite 550
Schaumburg, IL 60173
847-517-7225
www.smsna.org